Recognizing AIDS as an infectious disease
 Other
populations
Other
populations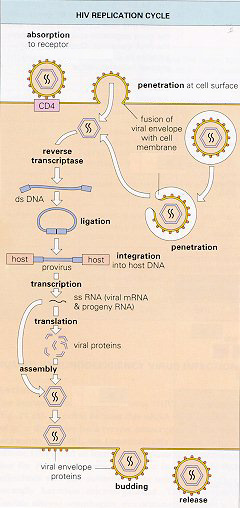
The appearance of AIDS in diverse populations implicated several routes
of transmission: anal and vaginal sex; contaminated needles; blood and
blood products, various fluid exchange points of mothers and infants, both
in utero and through breast-feeding.
In the United States, cumulative reports from the Center for Disease
Control and Prevention (CDC) indicate that 60% of adult AIDS cases were
sexually transmitted.
There are many factors that potentiate sexual transmission of HIV.
The most significant involve the transmission of bodily fluids in general.
Specifically penile penetration of the anus, relatively common among gay
and bisexual men, accounts for 53% of the 60% of sexually transmitted AIDS
cases. Penile penetration of the vagina is also a common source of transmission,
making up the other 7% of sexually transmitted AIDS. Other factors (such
as number of sexual partners, noninjecting drug use before sex, manual
trauma of the anus or vagina) are apparently relevant insofar as they increase
the likelihood of exposure statistically. However, it must be understood
that infection clearly relies on penetration and the transmission of fluids.
After much research it still remains uncertain what the likelihood
of infection is from any of the various oral sexual contacts. Generally
speaking, oral sex clearly is less likely to transmit the virus that causes
AIDS. There is nevertheless evidence to show that the risk of infection
through oral sex is not zero.
Needle-sharing is apparently a very likely way to transmit HIV. Injection
drug users (IDUs) are the second largest risk exposure category in the
CDC surveillance statistics. Through 1994, 32% of the AIDS cases reported
in the United States were associated with injection drug use. Consequently
there are probably 250,000 HIV positive IDU’s.
Almost half of the heterosexual women infected with HIV were apparently
infected by sexual contact with an IDU’s. In many parts of North America,
heterosexual injection drug users, their partners and their children, make
up the majority of newly reported cases.
There are other forms of transmission. During the early history of HIV, before blood products were properly testable, they were a common source of transmission. They made up a small but real part of all cases. Not only blood and blood products, but organs and skin grafts have caused infections. A few rare instances of transmission through biting and very unusual accidents have been shown. All of them have had actual blood to blood contact. There is no evidence to show that insect bites or casual contact carry any risk. Hugging, holding hands, and massage are all generally speaking safe. Deep kissing, although not totally ruled out, is an unlikely form of transmission at best.
Over time, we have learned that there are several stages to HIV disease.
The first is of course the actual initial infection with the virus. We
now know that at the time of infection there is generally a brief illness
(called acute seroconversion syndrome.) The symptoms usually occur 2 to
6 weeks after initial exposure to the virus. People report having fever,
lymph swelling, diarrhea, nausea; in general, they report cold like symptoms.
But then the illness passes, often going unnoticed, and HIV seems to go
into latency.
Indeed, the median time from initial infection with the HIV subtype
common in North America, to the development of what we call full blown
AIDS, is approximately 10 years.
Full blown AIDS is the point where the body begins to succumb, not
to the HIV, but rather to a slew of opportunistic infections, infections
that healthy individuals would conquer with their immune system. The rate
of disease progression from latency to mortality varies substantially.
Given this variability the question becomes: How do you measure the development
of HIV into AIDS? After that first “cold,” which seems to be defeated,
what happens? And how do you measure subsequent changes?
As the health care community has become cognizant of the risks of infection
with HIV (and other blood borne pathogens such as hepatitis B and C), various
techniques have been developed to prevent infection in clinical settings.
Because it was soon realized that health care workers would not always
know when a patient is infected, the CDC recommended the policy of ?universal
precautions.? Essentially these are precautions to prevent contact with
fluid thought capable of transmitting blood borne viruses; the word ?universal?
is meant to convey that blood, bodily fluids and tissues of all patients
are to be treated with precautions as if they might be infectious.
It should be noted that universal precautions (wearing latex gloves
for any contact with bodily fluids, washing hands before and after applying
latex gloves, disposing of all needles and potentially infected materials
properly, etc) serves not only to protect from infection. Persons with
compromised immune systems are more susceptible to all infections. Health
care workers must guard themselves from transmitting infections to the
HIV infected person. Universal precautions serve to protect the HIV infected
person as much as the non-infected person.
From a biological point of view, only one thing can prevent AIDS: preventing
transmission of HIV. One of the most important things to bear in mind is
that, although persons progressing to later stages of AIDS regain infectiousness,
newly infected persons are generally more infectious than persons infected
for a long time. This makes the visual appearance of a person practically
irrelevant in assessing infectiousness.
Before the isolation of HIV as the cause of AIDS, a diagnosis of AIDS
could only be based on a set of clinically diagnosed illnesses in the absence
of other known causes of immunosuppression. The reasoning went as follows:
“Here is an otherwise healthy person suffering from pneumonia, and/or Kaposi’s,
and/or some other illnesses (sudden weight loss, candida infection, etc)
that don’t usually strike people with healthy immune system. There is no
other explanation for their condition. Presumably, then, they are suffering
from AIDS, whatever AIDS may turn out to be.” Within this framework, a
comprehensive case definition was statistically worked out based on the
experience of medical providers.
With the recognition of HIV as the virus that causes AIDS it first became
possible to detect the infection. The bodies initial response to HIV is
the production of antigens designed to disable HIV. The first tests for
AIDS were actually such that, rather than testing for the actual presence
of the virus, an “enzyme-linked immunoassay” (ELISA) could test for the
presence of the bodies response. This first and still popular type of test
basically looks for certain antibodies which the body produces within weeks
of infection. This test could produce false positives and false negatives
under a variety circumstances, so it must be repeated, and checked after
several “positives.” The ELISA test was designed for sensitivity, not specificity,
so it has more false positives and fewer false negatives. But it allowed
for a rapid, reliable and inexpensive way to check blood and blood products.
After a few positive ELISA tests, testers turn to a far more sensitive
test to confirm infection. The mechanics of this test are significantly
more complicated, hence are also more expensive. The so-called “Western
Blot”, made of a crude version of HIV, is extracted from tissue culture
and laid out in parts on strips of paper. Again this test induces a reaction
from antibodies to HIV, but it produces more reliable results.
The procedure of choice for making an HIV diagnosis infection is a
demonstration of antibodies to HIV using an ELISA and a confirmatory Western
Blot. Methods for the direct detection of HIV are confined much to the
research area, due to their prohibitory cost. (See section on Viral Load.)
The expression of the disease depends on the condition of the patient
and the virus, and can be significantly altered by protective measures
and treatment. Its development is extremely variable. So one of the questions
researchers have wanted to answer for a long time is how do we assess where
someone infected with HIV is.
There is common surface receptor on many cells of the immune system
called a CD4 receptor. (Technically the cells are called a transmembrane
glycoprotein- a “T-cell.”) Certain things about the CD4’s of the body can
be easily measured and correlate strongly with the relative risk of development
of opportunistic infections or death. So the relative stage of a patient
can be assessed using this count of the CD4 cells. The CD4 counts have
some daily variability, and so are far from a perfect measure of AIDS,
but they have become an important way of tracking the disease’s progress.
We have general expectations of what T-cell counts (CD4 counts) to
expect (1000 per mm3 in healthy adults). Once this number drops below a
critical threshold (200 per mm3), there is a steep increase in the infections
associated with frank AIDS.
More recently, several studies have shown the importance of directly
measuring amounts of viral RNA (ribonucleic acid) in the blood plasma of
HIV infected individuals. With powerful new technology, we can detect the
minute quantities of this genetic material of HIV. This so called “viral
load” (sometimes called “viral burden”) is simply expressed as the number
of copies of HIV RNA per milliliter of blood plasma. Studies have shown
that this figure is actually a better predictor of the disease’s progression
than CD4 counts. The lower the viral load, the longer the survival time.
Armed with information about the amount of HIV in their blood plasma, individuals
will have a better way of deciding when and how to proceed with combination
therapy, to measure its success, and react to its failure.
Unlike T-cell counts (CD4 counts), for which we have general expectations
of what to find (1000 per mm3 in healthy adults), viral loads require a
series of loads to determine a baseline value for each individual.

Here is a list of the common nucleoside analogues:

A second major class of drugs have been developed which stop the action
of one of the enzymes that HIV uses in replication. The protease enzyme,
found in HIV-infected cells, cuts viral protein chains into useable lengths
for the production of new virus. The result is that the “protease inhibiting”
drugs results in the formation of defective HIV viruses that cannot infect
cells.
The most important thing to know about protease inhibitors is that
resistance and cross-resistance significantly complicate drug choice. HIV
develops resistance to anti-HIV drugs by changing its genetic material.
But HIV quickly develops resistance to all the known protease inhibitors
when they are used at doses lower than the recommended dose.
Cross-resistance is when resistance to one drug confers resistance
to another drug, even when that other drug has never been used before.
Cross-resistances are very common among the protease inhibitors.
The strategy of dispensing them depends very much on understanding
these resistances and cross-resistances. In general, this class of drug
is a powerful addition to our arsenal against HIV.

The major problem in producing clinically useful antiviral treatments
has been that available drugs have only achieved limited success in suppressing
viral reproduction. It has become clear that, even during asymptomatic
periods where the virus shows little signs of growth, there is extensive
replication of the virus in lymph tissue. And under the selection pressure
of antiviral treatment, mutations of the virus develop which are resistant
to the treatment used.
Faced with a collection of individual treatments, , none of which worked
perfectly (because they often culminated in resistant strains of HIV) it
was only a matter of time before researchers began giving more than one
drug at a time.
Although scientists prefer to use single treatment methods because two
or more drugs may have additive or synergistic interactions that are counterproductive
or unpredictable, sometimes two or more drugs work better than any drug
alone. Given that the HIV replication cycle offers several potential targets
for antiviral therapy, and given that we know that nucleoside analogues
and protease inhibitors work on different such targets, combinations of
the two suggested themselves. Research done in the mid-90’s showed that
certain combination therapies indeed produced dramatic reductions in HIV
replication and greatly reduced or slowed the development of frank AIDS.
On the basis of preliminary clinical trials, and these dramatic results,
multidrug combinations have become a significant weapon in our arsenal
against HIV.
It must emphasized that despite all the optimism generated by these
results, they are preliminary and far from perfect. Although, many people
have responded positively to combination therapy, we know that many develop
resistant strains that defy all know combinations. Moreover, the costly
regimens, with their multiple side effects, have been proven difficult
to sustain. And the problem of resistant strains makes it necessary to
decide carefully when to introduce what combinations, and in what order.
Finally, we must add that the researchers have no idea how long someone
can be sustained on these regimens. The drugs themselves are very new;
so the combinations with their synergistic effects, could very well prove
to have significant limitations beyond the ones already noted.

For the most part, antivirals have been used to treat people already clearly infected with HIV. There is some indication that it may be useful in preventing seroconversion in people who have been exposed to HIV. Essentially, the idea is to throw significant quantities of retrovirals at the HIV before it gets a chance to take hold in the cells of the body. . It has mainly been tested on people who have had quickly identifiable exposures. This is a very new area of research and it remains unclear what success can be had here

Treatments have been developed to cope with the illnesses which HIV
has promoted or even resurrected from near oblivion. Pneumocystis carinii,
one of the most common of pulmonary infections of HIV disease, has met
with recent advances in early detection, primary and secondary prophylaxis,
and aggressive treatment. Toxoplasma Gondi, an opportunistic infection
of the central nervous system, are also now more treatable than ever. Unfortunately,
with this infection, it is necessary to continue lifelong treatment. Several
infections of the digestive tract, especially Cryptosporidiosium, may be
more difficult to cure, but generally react well to the symptom directed
treatment that can control the diarrhea. Some of the life-threatening,
but many of the discomforting fungi, are generally treatable. The dangerous
meningitis and the more benign Candida respond to prophylaxis and/or antifungal
treatment. The worldwide epidemic of HIV infection has resulted in a major
secondary epidemic of the Mycobacterium tuberculosis. Although this illness
has remained more or less treatable by antimicrobials, there is apparently
an increase in the number of resistant strains. The implications of drug-failure
here are forebodingly profound. Similar treatments, with similar limitations,
exist for the family of herpes viruses (which includes, not only herpes
simplex and cytomegalovirus, but the herpesvirus associated with Kaposi?s
sarcoma.) Systematic chemotherapy has proven useful in dealing with many
presentations of Kaposi?s. The treatment of various lymphomas and cancers,
depending on the overall health of the infected, and the stage of HIV disease
involved, a variety of cancer treatments are available. Finally, there
are illnesses expressed in the central and peripheral nervous system, most
notable are peripheral neuropathy (commonly experienced as pain in the
extremities) and AIDS-related dementia (a persistent decline of cognitive
ability, sometimes leading to very prominent mental slowing and muscular
incoordination.) Infectious diseases, some of which have already been discussed,
may cause both of these. They also may be in some way related more directly
to HIV disease. In any case, they invoke for many the more frightening
medical conditions provoked by AIDS.

There are a number of areas, beyond antiviral combinations, being researched
at this time. Many of the promising directions, like pooled immune plasma,
Interferon, Interleukins, or the adoptive transfer of immune cells involve
various ways of boosting the body’s ability to produce its own immune response.
Perhaps someday a vaccine will prevent seroconversion in the first place.
Surely more promising breakthroughs on many fronts are coming our way.
But the future can be a very long time. Too long for some, so in the
absence of a full cure, we must do out part to treat, prevent and educate
today. For some, the future must be now.